Diabetic Retinopathy

What is Diabetic Retinopathy?
Do you have diabetes? You’re at increased risk of developing an eye condition called diabetic retinopathy. The eye doctors at North Georgia Eye Associates treat this and other eye conditions to ensure your eyes stay healthy.`
Diabetes is a condition in which the body’s ability to process and store sugar has been impaired. Among the characteristics of the condition are gradual changes in blood vessels.
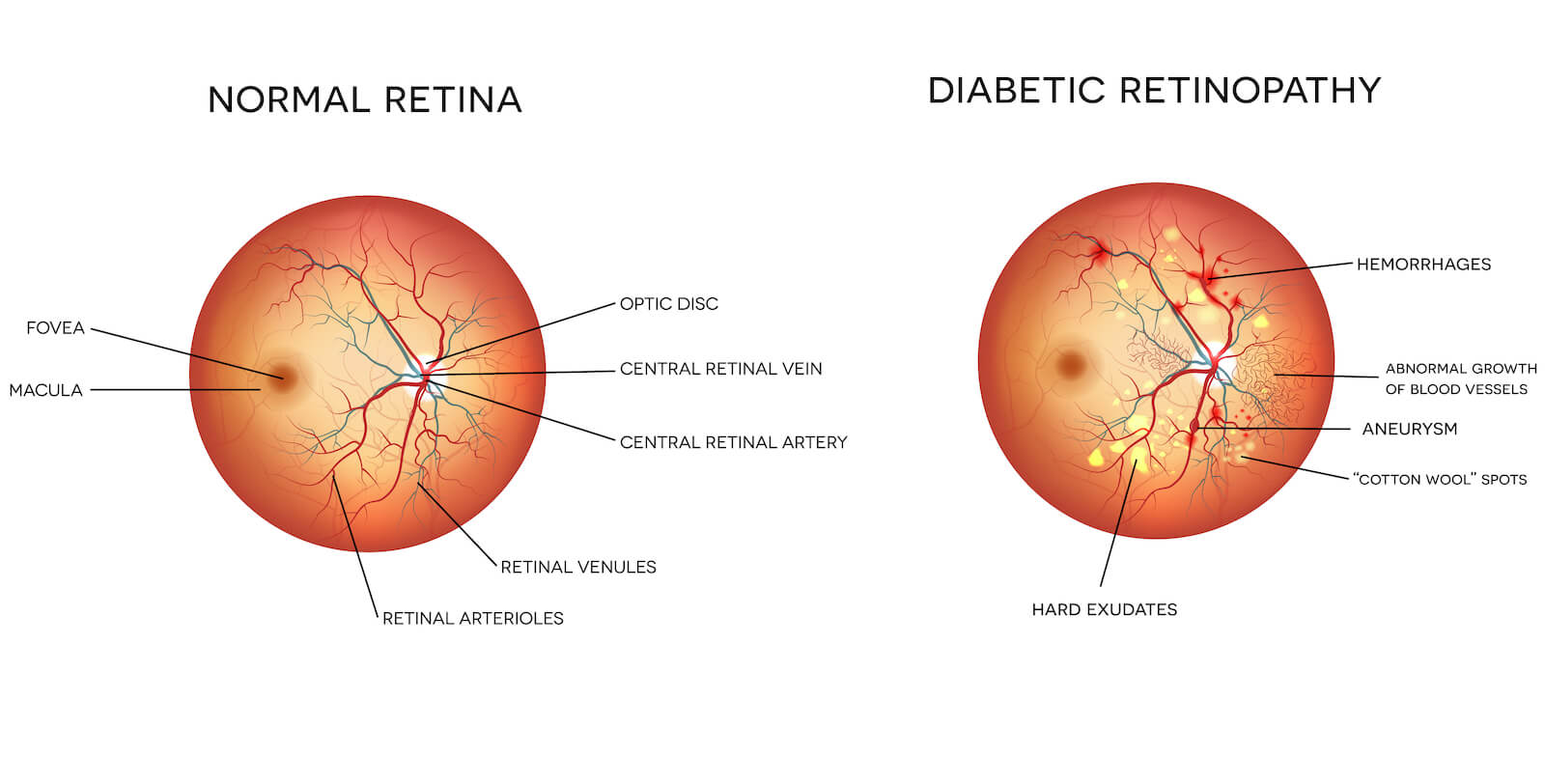
Diabetic retinopathy is a complication of diabetes caused by the deterioration of blood vessels nourishing the retina at the back of the eye. These blood vessels become damaged due to persistently elevated blood sugar. The damaged blood vessels can leak blood and fluid, resulting in retina swelling. This swelling can lead to permanent visual loss.
Who Is at Risk?
Persons who have had diabetes for many years are especially at risk of developing diabetic retinopathy. However, some patients can have evidence of diabetic retinopathy when first diagnosed with diabetes.
Six in ten who have had diabetes for over 15 years show symptoms of retinal damage; high blood pressure and pregnancy worsen the condition. Although your North Georgia Eye Associates ophthalmologist can easily detect diabetic retinopathy during routine eye examinations, it is the leading cause of new blindness among adults. It is treatable with laser surgery in the early stages.
People with diabetes are 25 times more likely to become blind than those without the condition, making eye exams especially important for patients with diabetes.
Two Types of Retinopathy
The two types of diabetic retinopathy are background retinopathy and proliferative retinopathy. In background retinopathy, blood vessels weaken and leak blood and serum.
These fluids collect and form deposits in the retinal tissues, causing them to swell. If the leaking blood vessels are in the peripheral area of the eye, no serious visual impairment usually occurs. However, if the fluid collects in the macula, blind spots and blurred vision can make reading and driving difficult or impossible.
Proliferative Retinopathy
In the second and more advanced stage of diabetic retinopathy, the abnormal cells rapidly spread (proliferate) across the retina’s inner surface. These weakened vessels can bleed into the vitreous and stop light from reaching the retina.
In addition, the connective scar tissue, which forms due to the ruptured blood vessels, can shrink. When this happens, it pulls the retina away from its underlying structure and causes it to detach. Severe loss of sight and even blindness may result.
What to Look For
There is no pain associated with either form of retinopathy. Gradual blurring of vision may occur. However, changes in the eye can go undetected without a medical eye exam.
When bleeding occurs in proliferative retinopathy, the patient may see spots, a clouding of vision, or experience a complete loss of sight in the affected eye.
Detection and Diagnosis
Eye doctors use numerous instruments and techniques to examine the retina. The critical point is that every person with diabetes needs an annual eye exam to screen for diabetic retinopathy. The exam typically takes about 10 minutes and involves dilating both eyes.
Treatment of Retinopathy
The eye doctors at North Georgia Eye Associates have extensive experience in diagnosing and treating diabetic retinopathy. We consider your age, medical history, lifestyle, and damage to the retina before recommending the appropriate treatment or intervention.
In many cases, treatment is unnecessary; in others, we may recommend laser treatments to halt further disease progression. These laser treatments can be performed in our state-of-the-art office facilities.
The laser procedures typically take 10-20 minutes to perform. In cases of background retinopathy, the laser is focused with pinpoint accuracy on the damaged blood vessels. The heat from the laser seals the blood vessels and helps bond the retina to the back of the eye by forming small scars.
One standard treatment for proliferative retinopathy is called panretinal photocoagulation. In this procedure, the peripheral retina is scattered with laser light beams, like the pattern made by a shotgun. Although a certain amount of healthy tissue is destroyed, this technique usually stops further growth of abnormal cells and preserves the macula, saving valuable straight-ahead and color vision.
Removal of the Vitreous
If the vitreous has become too clouded with blood to clear on its own, a surgical procedure called a vitrectomy may be recommended by your ophthalmologist. In this technique, the vitreous is drained and replaced with a clear, artificial solution. An immediate improvement in sight is noted in about 70% of cases.
Retinal Detachment
Retinal detachment occurs when the retina’s transparent layer separates from the eye’s wall. As the retina separates away, vision becomes darkened and distorted. Complete detachment leads to total loss of vision. Retinal detachment typically requires a vitrectomy or scleral buckle surgery to re-attach the retina.
If you have diabetes, your eyes are at risk for diabetic retinopathy. Early detection and diagnosis of diabetic retinopathy is vital if good vision is to be maintained.